Student: Is the “Clustering of Dyspnea Symptoms” done statistically or phenomenologically?
Professor: Both!
According to Lansing, Gracely, and Banzett (2009),
“There are at least three separable ‘qualities’ of uncomfortable breathing sensations”:
- ‘Work’,
- ‘Air hunger’, and
- ‘Tightness’.
“The division into different kinds of sensation classification is not based on perceptual quality alone. To be classed as distinct, the perception must have a different afferent source; this is most easily demonstrated by applying stimulus combinations that excite different afferents demonstrating that the sensations can vary independently.”
Sense of Work / Effort
Student: I can sense that this is like, “Breathing is hard work.” Or, “I am huffing and puffing to get up this hill.”
Professor: Try up a moderate hill in the mile-high city of Denver.
- No change in work capacity, said the classical physiologists.
- However, for me, all of a sudden part way up that hill, I was shocked with having to breathe harder than I would at sea level.
Professor: Lansing et al. (2009) state:
“‘Work’ of breathing is perceived as uncomfortable when the work of breathing or the required motor command:
- is increased by high minute ventilation (rate or tidal volume),
- by increasing impedance to inspiration,
- by weakness of respiratory muscles, or
- by placing inspiratory muscles at a disadvantageous length.
“Subjects and patients choose descriptors such as ‘my breathing requires more work’, ‘my breathing requires more effort than usual‘.”
Professor: Banzett (2007) summed up the mechanism for panting:
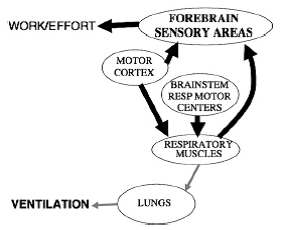
- “The neural pathways proposed for these sensations include corollary discharge from motor cortical centers that drive voluntary breathing.
- “Muscle mechanoreceptors and metaboreceptors are probably also involved, while corollary discharge from the brainstem is probably not (Figure 4).”
Figure 4. Neural pathways underlying work/effort sensation.
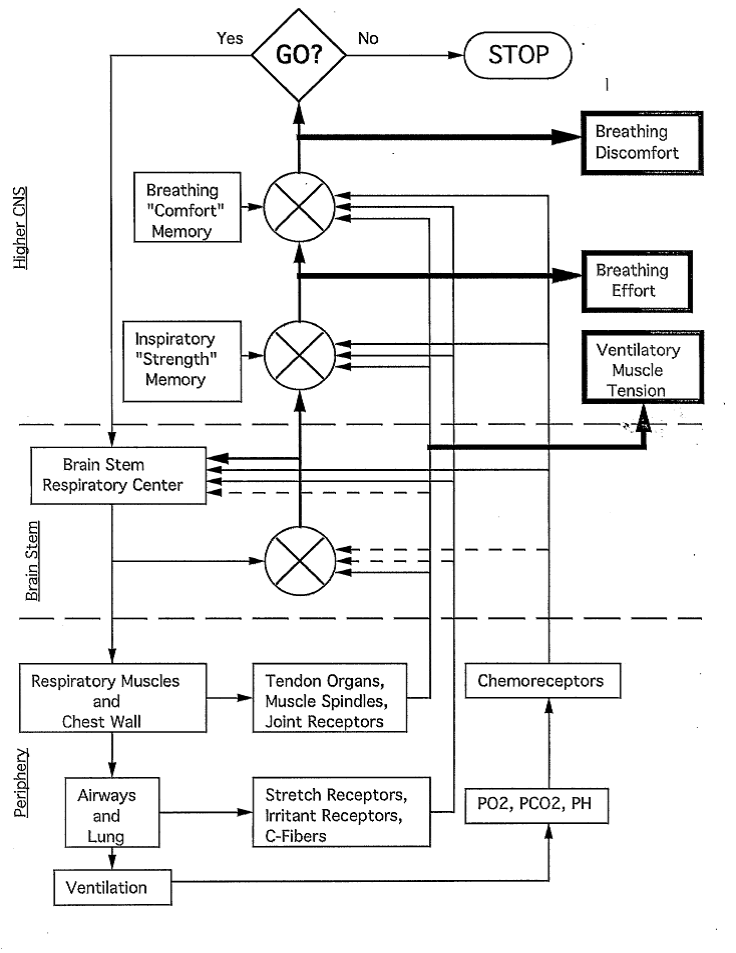
Professor: Hey, I found a preliminary figure for the Pulmonary Rehab book chapter (1993), and it looks very similar to Banzett (2007) Figure 4:
Figure: Schematic diagram of the mechanism for dyspnea, demonstrating the interrelationships among ventilatory muscle activity, pulmonary mechanics, breathing effort, and breathing discomfort.
Student: Wow! They are very similar, and yours was done 14 years earlier.
Air Hunger
Professor: Well, let’s move on to symptoms like, “I cannot get in enough air”. Or, “I’m starved for air.” Just picture a runner at the finish line, gasping for breath.
Professor: Moreover, Lansing et al. (2009) state:
- “‘Air hunger’ is the conscious perception of the urge to breathe, a fundamental biological drive. This sensation arises when pulmonary ventilation is insufficient.
- “It is described as ‘cannot get enough air’, ‘uncomfortable urge to breathe’, ‘starved for air’ and is the sensation felt at the end of a long breath hold.”
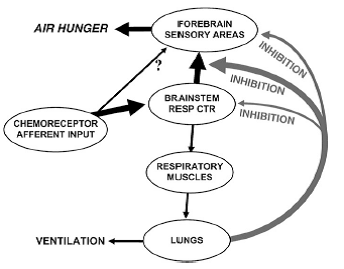
Professor: Banzett (2007) summed up the mechanism for not enough air:
- “The most likely afferent stimulus for air hunger is corollary discharge conveying a copy of the medullary respiratory center discharge to the sensory areas of the forebrain, although a role for direct projection of chemoreceptors to the forebrain has not been disproved.
- “We conclude that pulmonary stretch receptor information is capable of relieving air hunger; chest wall afferent information probably has a weaker effect. There is some information from animal experiments that suggests this inhibition takes place at a level above the medullary respiratory centers, but below the cortex (Figure 3).”
Figure 3. Neural pathways underlying air hunger. Proposed pathways for relief of air hunger by tidal inflation are shown by right hand arrows.
Professor: Please note that Air Hunger symptoms can be experimentally dissociated from reports of uncomfortable respiratory Work or Effort.
Chest Tightness
Student: And I have exercise-induced asthma that really makes me fight for breath.
Professor: Lansing et al. (2009) state:
- “‘Tightness’ appears to be specific to bronchoconstriction and is the earliest symptom of asthma.
- “Asthmatics report descriptors such as ‘my chest feels tight’ or ‘my chest is constricted’ localized to the chest or lungs.
- “Tightness is not the only sensation reported in asthma; asthmatics also report work and air hunger during severe attacks.”
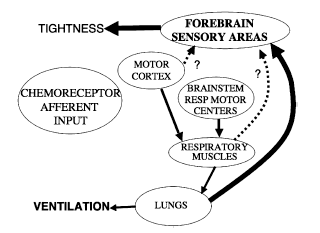
Professor: Banzett (2007) summed up the possible bronchoconstrictor mechanism for chest tightness:
“That the pathway for tightness [may also well be] vagal in origin (Figure 5).”
Figure 5. Neural pathways underlying tightness.
Student: Look at the three Figures from Lansing et al. (2009). They indicate feedback going to the forebrain sensory areas.
Professor: Very interesting! Let’s look into the studies of “corollary discharge conveying a copy of the medullary respiratory center discharge to the sensory areas of the forebrain.
Student: How about the emotional dimension of chest tightness and other breathing symptoms?
Professor: Okay.
Take Home Message: Uncomfortable breathing is reported as a mismatching of signals from ventilatory drive or airway with the resulting ventilation or discomfort memory,
Next: Cortical and subcortical central neural pathways in respiratory sensations (Davenport & Vovk (2009) Resp Physiol Neurobiol 167: 72–86).
References
Banzett RB. (2007) The peripheral mechanisms of dyspnea. pp 150-151, In: O’Donnell DE, Banzett RB, Carrieri-Kohlman V, Casaburi R, Davenport PW, Gandevia SC, Gelb AF, Mahler DA, Webb KA. (2007) Pathophysiology of Dyspnea in Chronic Obstructive Pulmonary Disease: A Roundtable. Proc Am Thorac Soc 4: 145–168.
Davenport FW, Vovk A. (2009) Cortical and subcortical central neural pathways in respiratory sensations. Resp Physiol Neurobiol 167: 72–86.
Lansing RW, Gracely RH, Banzett, RB. (2009) The Multiple Dimensions of Dyspnea: Review and Hypotheses. Respir Physiol Neurobiol 30: 53–60.
Parshall MB, Manning HL, Bourbeau J, Calverley PM, Gift AG, Harver A, Lareau SC, Mahler DA, Meek PM, O’Donnell DE. (2012) An official American Thoracic Society statement: Update on the mechanisms, assessment, and management of dyspnea. Am J Resp Crit Care 185: 435-452.
Weiser PC, Mahler DA, Ryan KP, Hill KL, Greenspon LW. (1993) Clinical assessment and management of dyspnea. In: Pulmonary rehabilitation: Guidelines to success. 2nd edition. Hodgkin, J, Bell CW, eds. Philadelphia: Lippincott, 478-511.